The functional medicine and larger holistic health community have been talking about “leaky gut” for the last few decades! Unfortunately, the conventional medicine community at large has looked down on this concept, with often knee-jerk responses.
This ultimately led to the rise of the term “intestinal permeability” to be more technical. Interestingly, the term “leaky gut” is making a comeback even in conventional biomedical research!
Today, research is consistently revealing that “leaky gut” is indeed a phenomenon that is running rampant in the US population. It is associated with many chronic illnesses and even conditions outside the digestive tract, including autoimmune conditions, obesity, heart disease, food sensitivities, and irritable bowel syndrome (IBS), and many more conditions!
In my functional medicine practice, I see leaky gut as a confounding factor in many patients’ chronic health complaints. As the research grows exponentially in the role of the gut in immune function, metabolism, the gut brain connection, protection from inflammation, and of course nutrient digestion and absorption, validation of each patient’s experience is common!
I hope this post is intriguing, and if you’re a budding gut health enthusiast, this one’s for you! Gut health is central to functional medicine and Chinese medicine alike, so it’s easily become a foundational focus of my practice! Let the world within each of us unfold!
In this post, we will dive into better understanding leaky gut, the fascinating structure of the gut, and discuss causes and signs of leaky gut. I will be using both terms, leaky gut and intestinal permeability interchangeably!
Here we go!
Structure of A Normal Intestinal Barrier vs. Leaky Gut
Our digestive tract is fascinating. If you’ve explored the realm of gut health, you’ve probably come across information about a plethora of topics – the gut/brain connection, the gut/immune connection, the microbiome, digestive enzymes, prebiotics, probiotics, and post biotics – the list goes on of course!
For the purpose of this post, we’ll draw attention to the lining of our digestive tract, specifically in the intestines. Normally, both our small and large intestines are composed of a lining that is a single-cell layer thick. These cells are joined together by proteins that are like the “glue” between these cells called “tight junctions.” (appropriately named, no?)
The integrity and strength of this single layer of cells lining the intestines and the tight junctions is incredibly important for many reasons, including the following:
- It’s a barrier that serves a main immune purpose of keeping pathogens that we eat and that may live in our microbiome out of the bloodstream
- It keeps larger, undigested food particles out of the bloodstream
- Being a single-cell thick allows for the diffusion of nutrients and water across the intact cells and into our bloodstream
The small intestine is the main site where we absorb most of our nutrients from food and drink into our bloodstream. The large intestine is the main site where we absorb water and some electrolytes into our bloodstream – and it houses a majority of our microbiome! Combined, the intestines are between 27-31 feet long in the average adult!
Leaky gut or intestinal permeability results when these tight junctions are loosened, damaged. Your gut is constantly regulating the opening and closing of these gaps, but when they become damaged it opens the potential for immune compromise, letting in food antigens, or improper nutrient absorption. Think of leaky gut as a continuum of potential leakiness and increased permeability.
Can you see how this can be a problem for the immune system?
What Causes Leaky Gut (Intestinal Permeability)
Naturally, you’re probably wondering, “well what causes leaky gut in the first place?” I would summarize the main causes as an unfortunate product of the many modern conveniences of our world. Go figure, right?
Here is a list of a dozen factors that contribute to leaky gut:
- Inflammatory foods and the Standard American Diet (SAD)
- Stress in its many forms
- NSAIDS, antacids, and antibiotics
- Oral contraceptive medication
- Environmental toxins such as heavy metals and pesticides
- Artificial sweeteners
- Alcohol consumption
- Chronic infections including parasites and H. Pylori infections
- Micronutrient deficiencies including zinc, vitamin D, and glutamine
- Too little sleep
- Smoking
- Overexercise
- Inflammation in its many forms
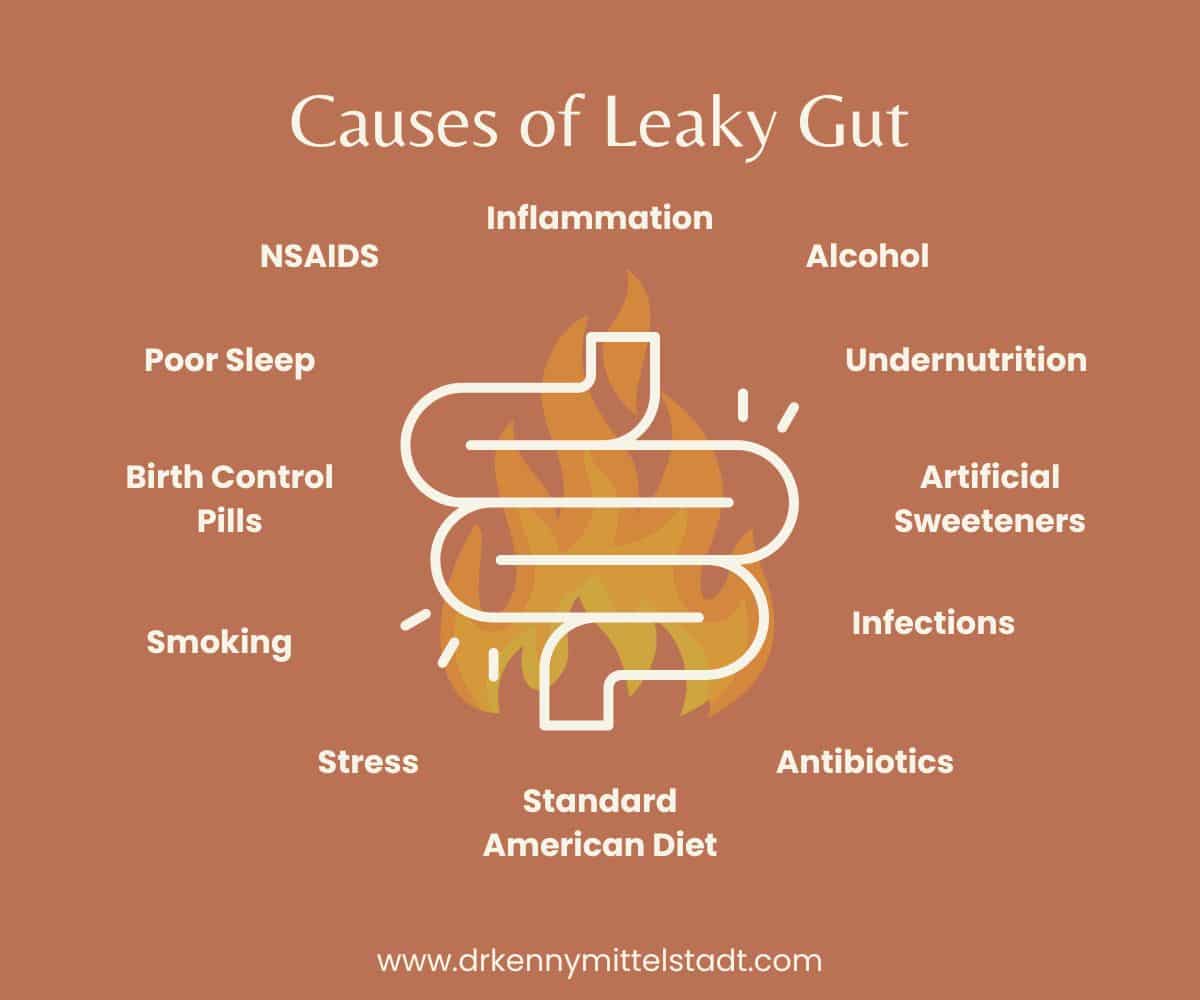
This is a list of some of the most common underlying causes of intestinal permeability. Each of these factors contributes to the loss of integrity of our ever-important single cell-thick barrier and the tight junctions and can set the body up for inflammation and even autoimmune reactions.
Perhaps one of the most interesting factors that may increase intestinal permeability is stress, even in the short term. Cortisol, one of our primary stress hormones, is a catabolic hormone, meaning it breaks things down in our bodies. One such target is actually our gut lining! In fact, elevated cortisol can signal our bodies to leach proteins from tissues throughout our body, including from the gut!
Signs and Symptoms of Leaky Gut (Intestinal Permeability)
The ways that “leaky gut” can manifest is unique to each person and varies greatly. Some individuals won’t experience stark symptoms, and this is part of what makes it so insidious and challenging to identify and treat.
Even if you don’t have physical symptoms, the loss of integrity of our intestinal barrier likely contributes to chronic, low-grade inflammation and heightened immune response that can manifest in chronic disease down the road. It’s subtle in many ways. See how tricky it is to inspire awareness and change?
However, many people do experience symptoms with intestinal permeability. You may think the symptoms might be limited to digestive symptoms, but this is not the case! Symptoms may be in the digestive tract or systemic, meaning throughout the entire body, and any combination of these!
Some of the most common digestive symptoms of leaky gut include the following:
- Constipation, loose bowel movements, or alternating symptoms
- Bloating
- Abdominal pain or cramping
- Gas pain and production
- Weight loss or weight gain
Some of the most common systemic symptoms of leaky gut include the following:
- Joint pain
- Fatigue and brain fog
- Feeling “Tired but wired”
- Depression and/or anxiety
- Skin problems
- Allergies & food sensitivities
- Low immunity, frequent colds and illness
- Thyroid dysfunction
- Headaches
- Fibromyalgia
- Recurrent urinary tract infections (UTI’s)
Quite the list of potential manifestations, eh? This is why the spotlight in health creation is on gut health. This has been a central tenet of Chinese medicine for thousands of years and continues to be so in the functional medicine space.
Even conventional medicine is beginning to recognize the importance of gut health and integrity of the lining to promote healthfulness throughout the entire body.
How to Test for Leaky Gut
There are many ways to test for intestinal permeability, some more specific and sensitive than others. Some tests may suggest the presence of leaky gut, while others can analyze it directly. Each option comes with pros and cons, limited sometimes by price, practicality, and sensitivity.
Here is a list and short description of 6 of the most common tests that are used for assessing intestinal permeability.
The Lactulose / Mannitol Test
This test uses two differently sized sugar molecules to test for whether or not the gap junctions are compromised. If too “loose” they may let the larger sugar molecule, lactulose, through the gut lining ultimately to be measured in the urine.
Zonulin Testing
Zonulin is one of the proteins involved in regulating the opening and closing of our tight junctions. It can be measured in the blood and stool, and elevated levels may suggest increased intestinal permeability.
Biopsy of the Intestines
Taking an actual tissue sample of the intestinal lining and analyzing it under a microscope is another method to look at signs of inflammation, damage, or loss of integrity of the tight junctions.
Testing for LPS in the Blood
LPS, or lipopolysaccharide, is a toxin that is produced by some “bad bacteria” in the gut. Elevated levels in the blood can indicate a compromised intestinal barrier.
Comprehensive Stool Test
Though a functional medicine stool test doesn’t test directly for intestinal permeability, it does reveal insight into related factors such as intestinal inflammation, microbiome diversity, the presence of pathogens, and the immune response within the gut itself.
Food Sensitivity Testing
Having many reactions or intense reactions with food sensitivity testing doesn’t directly measure leaky gut. But it is suggestive that intestinal permeability might be present or a factor contributing to those sensitivities.
As always, it’s important to look at each patient as an individual when assessing labs. It’s critical to consider the big picture including symptoms, one’s individual history, along with the lab results. Overemphasis on lab findings alone can skew results and gives the imperfect, though meaningful test, too much power out of context.
I would definitely recommend working with a healthcare professional that specializes in any of these tests for more accurate assessment and treatment! If you’d like to learn more about functional medicine labs, read more here!
Treatment and Management of Leaky Gut
Just as there are many causes of leaky gut, there are also many ways to support and treat the integrity of your gut lining! If you look at the causes of leaky gut above, you can also use it to avoid triggers and to help treat leaky gut as well.
The two factors that matter the most when confronting leaky gut is to minimize existing inflammation and to promote repair of the gut lining. So the following treatments address these two factors!
Dietary Interventions
Since dietary stress is an underlying cause of leaky gut, it makes sense that this should be a primary treatment. Ultimately, our goal is to minimize the inflammatory load. A formal elimination diet is a well-studied, structured way to approach healing the gut and strengthening its immune response.
Eating anti-inflammatory foods and focusing on eating more plants are two great ways to support the healing of intestinal permeability. Specifically avoiding processed foods, sugar, alcohol, gluten, and dairy can reduce the inflammatory burden on the gut lining!
Lifestyle modifications
Managing stress through techniques like mindfulness, meditation, and regular, moderate-intensity exercise can also benefit gut health by reducing cortisol levels and promoting relaxation. Adequate hydration and getting enough sleep are essential for maintaining overall well-being and supporting the body’s natural healing processes.
Gut health supplements for leaky gut
Supplements can play a role in treating leaky gut as well. They focus on repair and reducing inflammation in addition to promoting microbiome balance. Supplements that may be considered based on your individual needs include the following:
- Probiotics
- Digestive enzymes
- Turmeric
- Zinc-carnosine
- L-Glutamine
- Deglycyrrhizinated licorice
- Marshmallow root
- Aloe vera
- And more!

I recommend working with a functional medicine practitioner to tailor supplement programs to your individual needs. The same thing doesn’t work for everyone because it depends on YOUR unique underlying cause or combination of causes.
Addressing underlying causes
Finally, it’s important to turn off the proverbial “inflammatory faucet” rather than just trying to mop up the floor of inflammation. There are a multitude of underlying causes that contribute to leaky gut as we explored above.
This is where comprehensive, lab-based functional medicine programs can be a huge game changer to developing a tailored treatment plan based on your unique situation.
The underlying cause may be a low-grade parasitic infection, microbiome imbalance, alcohol, overexercise, or a history of antibiotic usage, or any combination of these and other issues. Either way, functional medicine lab testing can help shed light and create strategic interventions!
As long as the underlying cause remains unaddressed, you can throw all the supplements and medications in the world at a condition such as leaky gut and may never see total resolution. This is a central idea in functional medicine.
Conclusion
In the ever-evolving landscape of health and wellness, the concept of “leaky gut,” or intestinal permeability, has sparked significant interest and discussion. Despite initial skepticism from conventional medicine, research is increasingly validating its importance, linking it to a myriad of chronic conditions beyond the digestive tract.
As a functional medicine practitioner, I witness firsthand the profound impact of leaky gut on patients’ health journeys and hope to underscore the need for greater awareness and understanding.
As we navigate the complexities of leaky gut, hopefully, you can see how crucial it is to embrace a holistic approach to treatment and management. From dietary interventions and lifestyle modifications to targeted supplementation and addressing underlying causes, each facet plays a pivotal role in restoring gut health.
My ultimate goal is to empower individuals to take proactive steps toward gut healing fosters resilience and to reclaim agency over their well-being – through the power of small decisions every day! Read more about my personal functional medicine philosophy!
If this information resonates with you, share with a loved-one or fellow gut health enthusiast! Follow me on instagram or subscribe to my mailing list below to stay tuned with exciting updates to my blog and functional medicine offers.
About the Author
Kenny Mittelstadt is an acupuncturist and functional health practitioner based in San Antonio, Texas. He is trained through the Institute for Functional Medicine and received both of his doctorate degrees with highest honors from Southern California University of Health Sciences. He focuses on empowering patients through creating opportunities for integrated understanding and personalized root-cause healing - starting with gut health and growing beyond!